1
/
of
1
kicanada
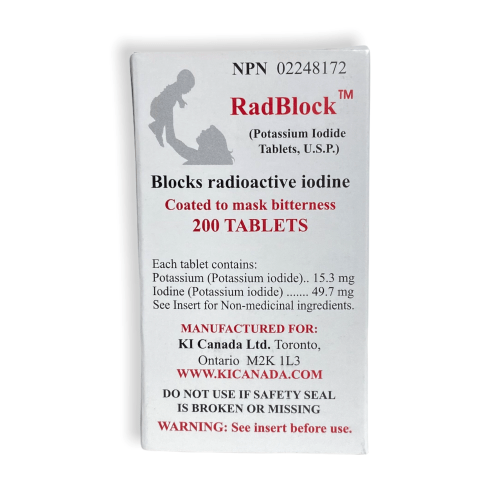
RadBlock 200 – Coated, Scored Potassium Iodide (KI) Tablets
RadBlock 200 – Coated, Scored Potassium Iodide (KI) Tablets
Regular price
$46.00 CAD
Regular price
$85.00 CAD
Sale price
$46.00 CAD
Unit price
/
per
Shipping calculated at checkout.
Couldn't load pickup availability
Share
FAQ
What is potassium iodide (KI) used for?
KI helps protect the thyroid from radioactive iodine during a radiation emergency, when directed by public health authorities.
How strong are these tablets?
Each tablet is 200 mg KI and is scored to help adjust dosing.
Who can take KI and how much?
Always follow public-health instructions. Dosing varies by age/weight and guidance.
Are the tablets coated?
Yes—coated for easier swallowing.
Storage & shelf life?
Store in a cool, dry place. Check label/package for expiration.
Is this medical advice?
No. Follow official guidance from public health authorities.

